Neck dissection (ND) is a complex surgical operation involving the removal of potential or proven metastases to cervical lymph nodes. The aim of the procedure is to remove lymph nodes from one side of the neck into which cancer cells may have migrated.
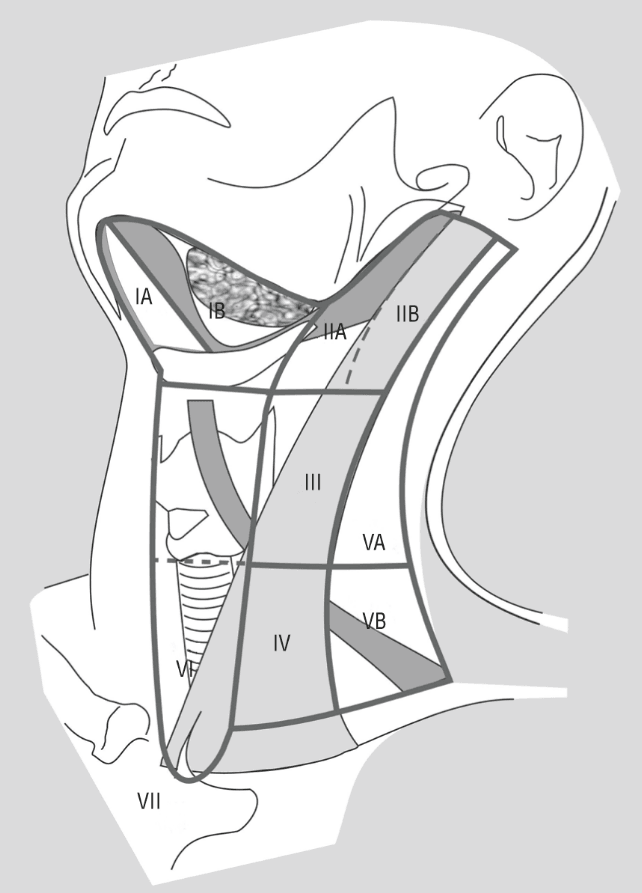
Prior to reading about the classification of neck dissections, knowledge about the levels of head and neck lymphatics, the drainage pattern of head and neck malignancies, etc is recommended.
Surgeons use different terms to describe neck dissections. Standardization of nomenclature and a proper classification of neck dissections would, undoubtedly facilitate inter-institutional communication, as well as the evaluation and reporting of treatment results when a given type of neck dissection is performed.

The current classification of ND is as per the Committee for Head and Neck Surgery and Oncology of the American Academy of Otolaryngology (2001). This is
- Comprehensive / Therapeutic neck dissection involves surgical clearance of Level I through V lymph nodes of one side of the neck, from the inferior border of the mandible to the clavicle, and from the anterior midline to the anterior border of the trapezius muscle.
- Radical neck dissection (RND) – This involves the removal of Level I-V lymph nodes with the removal of the spinal accessory nerve (SAN), Internal jugular vein (IJV) and Sternocleidomastoid muscle (SCM).
- Modified radical neck dissection (MRND): When modification of the RND involves the preservation of one or more non-lymphatic structures (SAN, IJV or SCM), the procedure is termed a modified radical neck dissection.
- Extended radical neck dissection (ERND): When the modification involves removal of additional lymph node groups or non-lymphatic structures relative to the radical neck dissection, the procedure is termed an extended radical neck dissection (ERND).
- Selective neck dissection (SND): When the modification involves the preservation of one or more lymph node groups that are routinely removed in the RND, the procedure is termed a selective neck dissection (SND).
Other classifications of neck dissections are Medina Classification and Spiros Classification.
Salvage neck dissection: This is a neck dissection done in a previously treated neck, whether previously treated by radiation, chemotherapy or surgery. This is performed for a persistent tumor in the neck lymph nodes despite treatment.
Radical Neck Dissection (RND)
This procedure was described by Crile in 1906 and later popularized by Hayes Martin in 1957.
Radical neck dissection (RND) involves en-bloc removal of Level I-V lymphatics with the removal of the spinal accessory nerve (SAN), Internal jugular vein (IJV) and Sternocleidomastoid muscle (SCM).
RND is the gold standard operation for metastatic neck diseases. All other procedures represent one or more modifications to this procedure.
Indications for radical neck dissection
Being a radical procedure associated with extensive morbidities, RND should be performed only in patients with malignant tumors of head and neck.
Following are the absolute indications for RND
- Significant operable metastatic neck disease with tumor bulk near to or directly involving SAN and/or IJV
- Extensive recurrent disease after previous selective surgery or radiotherapy.
- Clinical signs of gross extranodal disease
- Prior to a pedicled flap reconstruction – to reduce the bulk of flap in the neck and complete clearance of neck as re-addressing the neck later will be difficult with the flap pedicle.
Another relative (?controversial) indication for RND is an extensive primary lesion that is being treated surgically with an N0 neck, but where a pedicled reconstruction flap is needed.
Contraindications for radical neck dissection
Contraindications for radical neck dissections are
- When the malignant primary is untreatable.
- Patient unfit for surgery
- Those patients with distant metastasis except in differentiated thyroid cancers where RND is done prior to systemic treatment with radioiodine and external beam radiotherapy.
- Patient with significant bilateral disease – at least one IJV needs to be preserved.
- Unresectable disease in the neck like the involvement of the carotids, invasion of the prevertebral fascia and muscles along with the brachial plexus and extension onto and into the skull base.
Extended Radical Neck dissection
Extended Radical Neck dissection involves radical neck dissection with the removal of one or more additional lymph node groups or non-lymphatic structures or both.
The additional lymph node groups include suboccipital nodes, retropharyngeal nodes, parapharyngeal nodes, parotid nodes, facial nodes (e.g. buccinator nodes), or Level VI and VII lymph nodes. Non-lymphatic structures include mandible, parotid gland, part of the mastoid tip, prevertebral fascia and musculature, hypoglossal nerve, external carotid artery, vagus nerve, paraspinal muscles, and skin.
Indications for extended radical neck dissection
- When neck diseases invade any of the above non-lymphatic structures.
- When primary tumor arises in parotid gland or in the pharynx (may need retropharyngeal node clearance dissection)
- For transglottic and subglottic carcinoma larynx, carcinoma esophagus, carcinoma thyroid, etc, where it is necessary to remove paratracheal, pretracheal and anterior compartment nodes.
Modified Radical Neck dissection (MRND)
Modified Radical Neck dissection (MRND), described by Oscar Suarez and E. Bocca in 1967, includes the removal of all lymph nodes (level I-V) with the preservation of one or more non-lymphatic structures – spinal accessory nerve (SAN), Internal jugular vein (IJV) and Sternocleidomastoid muscle (SCM).
By preserving one or more of these structures, such modifications of the RND can preserve shoulder function, cosmetic appearance, and normotensive venous outflow, while still removed, comprehensively, are all the lymph node regions (I through V) of one side of the neck.
Depending on the non-lymphatic structures preserved a modified radical neck dissection can be classified into three –
| Types | Description | Indication |
| Type I | preserves SAN |
|
| Type II | preserves SAN, IJV |
|
| Type III | preserves SAN, IJV, SCM (also known as functional neck dissection) |
|
Selective / Elective neck dissection (END)
A selective neck dissection consists of the preservation of one or more lymph node groups (level I-V) and all three non-lymphatic structures with the removal of the cervical lymph nodes which are considered to be at high risk for metastasis from a given primary site. Selective neck dissection (SND) is done for N0 necks (no clinical evidence of neck nodes) or for very limited cervical metastases.
The principle of selective neck dissection is that in an untreated neck, patterns of lymphatic spread may be predictable and occult disease is usually found in the first echelon node.
The high incidence of occult metastasis in tumors of oral cavity, pharynx and to a lesser extent supraglottic laryngeal cancers, forms the basis of selective neck dissection.
Selective neck dissections are generally performed on an elective basis. END is indicated when the risk of having occult cervical nodal metastases exceeds 15-20%.
There is a big debate going on in the head and neck oncology group, regarding the role of END. Though the purpose of this article is not to debate the risk-benefit aspects of dissecting selected lymph node regions, a quick wrap up of these arguments in favor and against elective neck dissection are listed below-
Following are the arguments favoring END
- High incidence of occult metastasis in head and neck squamous cell carcinoma
- Limited neck dissection has low morbidity and mortality
- If the neck has to be entered to remove the primary lesion, it is better to perform elective surgery at the same time.
- By doing neck dissection, it is impossible to provide clinical follow-up necessary to detect the earliest conversion of the neck from N0-N1.
- Allowing neck metastasis to develop increases the incidence of distant metastasis.
- The cure rate for neck dissection is decreased when the neck becomes N+
- END can serve as a biopsy, helps in the pathological staging of the neck and can be an indicator of the risk of systemic disease.
- END can be performed during the primary surgery.
The opponents for END argues that
- Cure rates are no lower if the surgeon waits for the neck to convert from N0-N1
- Keeping the patient under close clinical follow-up will allow the earliest detection of N0-N1
- END results in a large number of unnecessary surgical procedures associated with inevitable morbidity.
- Radiation to the neck is as effective as neck dissection for N0
- END removes the barrier to the spread of disease and may have a detrimental immunological effect.
- Even if END acts as an indicator of systemic disease, there is no systemically effective treatment that can prolong disease-free interval in head and neck malignancies.
Indications for END for N0 neck are
- in oral cavity cancers, which include removal of levels I-IV. If END is performed, adjuvant RT should be considered if histopathologically any nodes come positive for malignancy.
- in laryngeal and hypopharyngeal cancers incidence of N0 neck is low and if the primary is treated surgically END needs to include level II-IV only.
Based on the levels of neck nodes removed, elective neck dissection can be further classified into
| Type of END | Nodal stations cleared | Major indications |
| Supra-omohyoid neck dissections | I-III | For Squamous cell carcinoma oral cavity |
| Lateral neck dissections | II-IV | Squamous cell carcinoma larynx, oropharynx, and hypopharynx |
| Extended Supra-omohyoid / Anterolateral | I-IV | Squamous cell carcinoma oral cancers Skin cancer (squamous cell carcinoma and melanoma) anterior to line of the tragus. Performed in conjunction with a superficial parotidectomy. |
| Posterolateral | II-IV + post auricular nodes | Skin Cancer (squamous cell carcinoma and melanoma) posterior to line of tragus. |
| Anterior or central | VI | Differentiated thyroid cancers, subglottic and hypopharyngeal squamous cell carcinoma. |
| Superior mediastinum | VII | Differentiated and medullary thyroid cancers Subglottic laryngeal and hypopharyngeal squamous cell carcinoma Cervical esophageal carcinoma |
Due to evolving practices, the 2001 AAOHNS classification omitted the named subtypes in favor of precise description with “SND” and parentheses denoting the levels removed, e.g. SND (I-IV).
References
- Ferlito A, Robbins KT, Shah JP, et al. Proposal for a rational classification of neck dissections. Head Neck. 2011;33(3):445-50
- Medina, J. E. (1989). A Rational Classification of Neck Dissections. Otolaryngology-Head and Neck Surgery, 100(3), 169–176.
- Robbins KT, Shaha AR, Medina JE, et al. Consensus statement on the classification and terminology of neck dissection. Arch Otolaryngol Head Neck Surg 2008;134:536–8
- Harris T, Doolarkhan Z, Fagan JJ. Timing of removal of neck drains following head and neck surgery. Ear Nose Throat J. 2011Apr;90(4):186-9