Total laryngectomy is a surgical procedure, most commonly done in cancers of the larynx (voice box). In this procedure, the entire voice box is taken off and a permanent hole (tracheostomy/stoma) is created in the neck, through which the patient respires for his entire life.
The indications, contraindications, surgical steps of laryngectomy are discussed separately in another article.
After a laryngectomy, the patient won’t be able to talk and communicate, which results in psychological, social and economic trauma. To overcome these various rehabilitation methods like esophageal speech, electronic larynx, tracheoesophageal prosthesis, etc are available.
This article describes voice rehabilitation after laryngectomy with help of a tracheoesophageal prosthesis (TEP).
Tracheoesophageal Puncture (TEP) Speech
The tracheoesophageal puncture was an anecdotal observation when a total laryngectomy patient had deliberately punctured the back wall of the trachea as he was trying to commit suicide. The patient used a heated ice pick through the tracheal stoma. He subsequently found that on occlusion of the stoma with a finger, exhaled air caused vibrations in the throat which could be articulated into speech.
In TEP, a fistula (passage) is created in the thick party wall separating the trachea (airway) and esophagus (food pipe) surgically. This surgical procedure can be done primarily, at the time of total laryngectomy, or secondarily at weeks or years after total laryngectomy. Several days after the puncturing of the tracheoesophageal party wall, a one-way valve prosthesis is placed in the track.
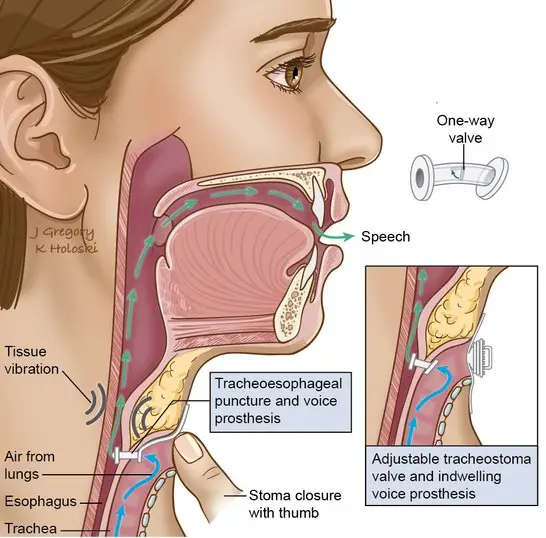
The tracheoesophageal prosthesis is a one-way valve that allows exhaled air from lungs to pass into the esophagus when the tracheostomy stoma is closed. This air enters the esophagus and escapes through the mouth during which it induces vibration of the pharyngoesophageal segment for sound production. For this a tonic pharyngoesophageal segment (also called PE-segment, neo-glottis or pseudo-glottis) is mandatory.
Advantages and Disadvantages of TEP Speech
Advantages
- Tracheoesophageal speech allows rapid restoration of voice after total laryngectomy.
- The sound is a natural one unlike the monotonous robotic sound with an electrolarynx.
- The air source is internal and needs no external device.
- The flow and pressure can be controlled by the patient, it allows “Normal” utterance length, improved fluency and duration of the speech. The speech has got increased acceptability, more normal phrasing with intelligible tonal language.
- If using an indwelling type of prosthesis, it has got minimal maintenance only.
- The current trend is to use hands-free occlusion for speech and moisture conservation devices applied to stoma – the device connected to the stoma has a valve within it. The valve allows smooth respiration, but not quick exhalation, as in speaking, redirecting air current through TEP.
- Moreover, the tracheoesophageal puncture is a reversible procedure.
Disadvantages
- For puncturing of the tracheoesophageal wall, surgery is needed, and the surgeon needs high training.
- The voice is slightly restricted in pitch range.
- Stenosis of the tracheostomy can make the placing of TEP difficult.
- Tracheitis, excessive secretions, wound healing problems, inaccurate sizing and puncture stenosis can lead to improper fitting of the prosthesis.
- Infection and fungal colonization of the prosthesis with Candida is a common problem. The newer Provox Activale claims to be Candida resistant.
- Periprosthetic (around the prosthesis) and intraposthetic leaks can occur which results in aspiration of liquids and pulmonary problems.
- Prosthesis degradation – The average lifetime of a voice prosthesis from insertion to replacement ranges between 4.7-8 months.
- The prosthesis may get dislodged accidentally – the patient may swallow it or inhale it into the lungs.
- The patient or relative needs to learn about removing, cleaning and re-introducing the prosthesis, which needs training and intelligence.
Candidacy criteria for TE Speech
When considering tracheoesophageal speech as the rehabilitation method post total laryngectomy, it is best to select people who meet following candidacy criteria.
- Highly motivated patient and caretaker
- Adequate patient understanding of post-surgical changes in anatomy and mechanics of voice prosthesis.
- Adequate cognitive ability
- Adequate dexterity and vision to take care of stoma and prosthesis.
- Patent stoma with adequate digital occlusion – more than 1.5sq.cm
- Passing insufflation test – ability to produce TE voice following esophageal insufflation via properly positioned esophageal catheter (the Taub test).
- Adequate pulmonary support
- With functional pharyngoesophageal segment
A tracheoesophageal prosthesis is not an option for the following type of patients.
- Significant stenosis of the hypopharynx.
- Increased pressures within the pharyngoesophageal segment
- Inadequate pulmonary reserve – those with COPD, emphysema, pulmonary fibrosis, interstitial lung disease, etc.
- Inadequate depth and diameter of the stoma to accept prosthesis without airway compromise.
Other modalities of rehabilitation like electronic larynx, esophageal speech, etc can be considered for failed candidates.
Primary Vs Secondary TEP
Primary TEP is the puncturing done along with total laryngectomy, while secondary TEP is done as a second surgery in a later stage. Regardless of whether the TEP is done primarily or secondarily, the basic principle is the same.
Primary TEP
Primary TEP is now accepted as the optimal method of voice rehabilitation because of multiple advantages (explained below).
Procedure:
- After a laryngectomy, a cricopharyngeal myotomy and a unilateral pharyngeal neurectomy are done.
- Opening on the posterior tracheal wall is made using a trocar, in a horizontal fashion to prevent a tear in esophageal wall, at a distance 5-8mm from tracheocutaneus junction proper visualization of the prosthesis for maintenance.
- It is preferred to put the prosthesis in a later stage. In such cases, a stent (size 12Fr) placed in the puncture. Some pass a feeding tube through the fistula (tracheo-gastric tube), which addresses the postoperative patient’s hydration and nutrition. At about 10 days after surgery /healing patient starts oral feeding, this can be removed, and a front-loading prosthesis can be inserted.
- Some surgeons prefer to insert the prosthesis immediately by pulling it into position using a flexible guidewire.
Secondary TEP
Secondary TEP is rarely practiced these days. But this can be considered in few selected patients like, those undergoing salvage laryngectomy (heavily irradiated larynx), those patients in whom pharyngeal reconstruction performed and patients in whom upper esophagus is resected and replaced with jejunum of the stomach.
Procedure
- The procedure can be done under local anesthesia or general anesthesia, but preferably under general anesthesia.
- A rigid bronchoscope (or esophagoscope/ hypopharyngoscope /pharyngoscope) that has a side opening near its distal end is introduced through the mouth into the pharynx and placed against the upper end of the membranous trachea which is punctured with a needle about 6-7mm from upper myocutaneous junction of tracheostoma.
- The puncture is dilated, and an indwelling prosthesis can be introduced by being pulled into place through the pharynx (rather than front-loading).
- Some use a stenting catheter (12Fr Foley) placed through the puncture into the esophagus. 4 days later catheter removed, length of prosthesis required is measured and the appropriate prosthetic valve is introduced.
| Primary TEP | Secondary TEP |
| Advantages | |
| The patient does not have to undergo secondary procedure/return to operation theater (including the related costs and risks) | Can be done in the clinic (Surgeon specific) |
| The rapid return of voice and rehabilitation can be started immediately | May promote more stability of TEP. |
| Ideal for primary total laryngectomy | It can be considered for salvage laryngectomy (radiated larynx) and other selected cases. |
| May allow for feeding through TEP site via a Ryles tube. | |
| Allows time for healing. | |
| Disadvantages | |
| Initial sensitive stoma | Rehabilitation will be delayed until TEP insertion done. |
| Post-op RT may delay speech | Two operations needed and the cost associated. |
| Dilation of the TEP due to the movement of the catheter | the greater voice failure rate |
| Migration of the TEP as healing progresses | |
Types of TE prosthesis
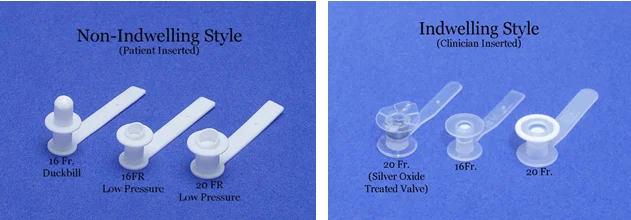
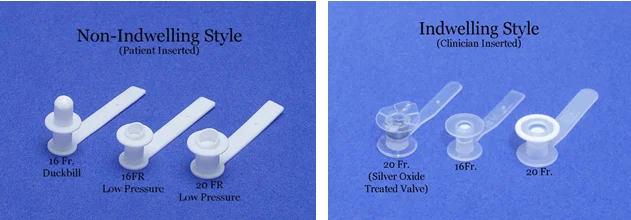
A tracheoesophageal prosthesis can be broadly classified into two types, patient inserted, or non-indwelling type and a clinician inserted or indwelling type. Differences between both types are summarized below.
| Non-Indwelling | Indwelling |
| Can be removed by the patient | Needs to be replaced by the clinician. |
| Daily maintenance includes cleaning & flushing | Robust construction i.e. longer life. |
| Need manual dexterity; Voice prosthesis has a strap and requires a piece of adhesive tape. | Success independent of patient age & general health |
| Less expensive | More expensive |
| E.g.: Blom-Singer Duckbill, Panje, | Blom-Singer Indwelling, Provox, and Provox 2, Groningen, VoiceMaster, Nijdam, Bordeaux, Groningen Voice Button |
Provox Vs BlomSinger Prosthesis
Among the available tracheoesophageal prosthesis, Provox and Blom-Singer are the most popular and commonly used ones. These features are described below.
Blom-Singer DuckBill Voice prosthesis
This is a patient maintained (non-indwelling) type of TE prosthesis with a one-way slit valve. The prosthesis is made of Silicone. The valve opens under positive pressure, and air from the lungs crosses into the esophagus to produce voice.
The diameter is 16Fr. and it’s available in lengths of 6mm to 18mm length.
Blom-Singer Indwelling prosthesis.
This is a clinician maintained one, which is available in two diameter sizes – 16 Fr. and 20 Fr and having lengths ranging between 4 mm to 22 mm.
The prosthesis can be placed primarily or secondarily. It is placed anterograde at the time of surgery. It has got a gel cap and a tubed loading system, with the delayed opening of the esophageal flange.
The prosthesis has silver oxide as a preservative.
Provox 1 Voice prosthesis
This is a low resistance, indwelling type of device, which can be placed primarily or secondarily. Its made of silicone, available in 6, 8 and 10 mm length. Its limitation is the retrograde insertion procedure.
Provox 2 Voice prosthesis
This is also a low resistance, easy to maintain prosthesis which allows both anterograde and retrograde insertion.
The prosthesis comes with a loading tool with the instantaneous opening of the esophageal flange.
The main advantage of this prosthesis is its radio-opaque nature which helps in detecting the device in case of accidental dislocation.
Provox Activale
This newer generation Provox prosthesis is made of candida resistant material. It also has magnets that are available in three opening forces, which prevents inadvertent opening of the valves.
Selection of prosthesis
The following parameters are generally taken into consideration when selecting the prosthesis.
- 16Fr. size prosthesis is considered at 1st fitting (some surgeons prefer 14 size). It is later dilated to 16 or 18Fr. depending on tissue integrity.
- Candidate dexterity – if the patient is willing to self-perform prosthesis changes, then a non-indwelling prosthesis is preferred.
- Phonatory effect – if the voice quality is effortless, loud and consistent, then the patient may do well with a higher-resistance device with increased durability. If the voice quality is strained and effortful, a lower-resistance device of greater diameter (20F) may be appropriate.
- The thickness of the party wall – The thickness of the tracheal wall varies from person to person and the length of the prosthesis needed should be accurately calculated. A too-long prosthesis will cause a ‘pistoning effect’ and consequently leakage around the prosthesis, while a too short prosthesis may result in aphonia.
- Durability – If the device recurrently leaks in less than a couple of months with no treatable cause, a device with higher resistance and durability should be considered. On average, a prosthesis lasts for about 4.8-6 months.
- Cost – cost issues should be considered when devices are comparable in style and performance.
Post TEP insertion care
After TEP insertion, the patient and family need to be taught on how to clean, change and manage the prosthesis, as well as how to use a prosthesis to speak.
The mucus from the face of prosthesis needs to be removed regularly. A cleaning brush and flushing tool can be used to clean the voice prosthesis at least twice daily.
Speech therapy should be initiated and continued after TEP insertion until patients speaking/swallowing is sufficient. Speech therapy after primary TEP is found to be better than one after secondary TEP. Direct speech therapy should involve;
- Valving – closure of stoma with a finger, thumb or outer valve to direct the air for speech
- Articulation – shape, and speed of lip, teeth and tongue movements
- Rate – of speech
- Phrasing – co-ordination of closure/opening of tracheostoma with onset to/stopping of voice
- Improving pitch, intensity, and suprasegmentals.
Complications & Troubleshooting of TEP
TEP insertion is associated with some complications like infections, leaks, extrusion, etc. Complications and troubleshooting of Tracheoesophageal prosthesis are considered separately in another article.
References
- Watson JB, Williams SE (August 1987). “Laryngectomees’ and nonlaryngectomees’ perceptions of three methods of alaryngeal voicing”. J Commun Disord. 20 (4): 295–304
- Singer MI, Blom ED. An endoscopic technique for restoration of voice after laryngectomy. Ann Otol Rhinol Laryngol. 1980 Nov-Dec;89(6 Pt 1):529-33
- Stephen J. et al. The Singer-Blom Voice Restoration Procedure. Arch Otolaryngol. 1981;107(11):674-676